
Skin Allergy Testing
This is less invasive than blood tests and is a good alternative for patients who don’t like needles.
learn moreNearly one-third of adults had a seasonal allergy, eczema, or food allergy.
*According to the CDC.

An allergy is the immune system’s reaction to a substance that it misinterprets as a threat. The immune system goes on the defense, producing antibodies that travel to cells throughout the body, while releasing histamines that result in an allergic reaction.
Allergies are the world’s most common chronic condition. In the United States alone, allergies are the sixth leading cause of chronic illness. They can cause reactions that range from mildly uncomfortable to life-threatening, according to the Asthma and Allergy Foundation of America.
For many allergies, you can limit your exposure to allergens by staying away from certain places or following certain rules. But if you have an allergy to something like insects or pollen, you can’t always avoid being exposed to it.
Our bodies interact with allergens on a regular basis. Under normal circumstances, the body does not have a pro-inflammatory response, resulting in what is known as a Type 1 immune response.
But in people with allergies, the body switches to a Type 2 immune response when confronted with the allergen.
In a Type 2 immune response, the immune system sends in T helper type 2 cells, which results in the production of immunoglobulin (Ig) E molecules that trigger the production of histamines and other chemicals.
Allergic sensitization occurs when the body is first exposed to an allergen and a Type 2 immune response.
Through this process, the body “learns” to recognize the allergen. As a result, the next time the body is confronted with the allergen, it is ready and waiting to initiate the inflammatory response.
There are many different types of allergies, each triggered by its own allergen or category of allergens. The following are some of the most common allergies:
There are some common symptoms associated with allergies, but signs and symptoms of allergies will vary from patient to patient and may depend on the type of allergy involved.
For example, a latex allergy might create a skin response while a pollen allergy will generate respiratory symptoms.
People with allergies can have different general signs and symptoms. These are some of the most common signs of allergies:
People with allergies can have different general signs and symptoms. These are some of the most common signs of allergies:
In severe cases, a patient will go into what is known as anaphylaxis. This is a life-threatening, severe allergic reaction that can cause your body to go into shock.
Anaphylaxis requires immediate medical intervention because, as a result of shock, your blood pressure can drop suddenly and your airways can narrow, impacting breathing.
Usually, anaphylaxis symptoms impact more than one organ system, ranging from the lungs and heart to the gut.

While COVID can include some of the same respiratory symptoms as some allergies, it also comes with several other symptoms typically that are not present in allergic reactions.
These include fever and chills, muscle and body aches, and new loss of taste or smell. It may be difficult to tell the difference between allergy and COVID-19 symptoms at the height of allergy season.
Consider your personal medical history with allergies before assuming that you might have COVID-19. Testing can help give you more definitive answers on whether you’re experiencing allergies or COVID-19.

When you have asthma, a cold, or bronchitis, the symptoms can be very similar, making it hard to know which type of doctor to see.
Asthma tends to last longer than the other types and can be caused by allergens, things that irritate the airways, like smoke, or infections.
Because the differences between these conditions can be hard to tell apart, it is often best to see a specialist. Allergists at AllerVie Health can give you accurate diagnoses and treatments that go beyond what a primary care doctor can do.
Our allergists treat allergies, asthma, and related conditions. They also have the equipment and capabilities to perform tests used to diagnose these conditions and then are able to develop treatment plans based on the results.
Make an AppointmentAllergies and asthma are sometimes a package deal that come in the form of allergic asthma. This happens when allergens trigger asthma symptoms—one of the most common occurrences.
The following are some of the common symptoms of allergic asthma:
The following are some of the more common triggers for allergic asthma:

In people with allergies, their body views allergens, such as pollen and dust mites, as a potential threat—even when they aren’t.
The body’s immune system takes over and produces antibodies to fight what it thinks are “harmful” allergens. An allergic reaction, which can include itching and sneezing, is how a body responds to an allergen.
There is a genetic component to allergies. Children who have one parent with allergies are 50% more likely to have allergies; that probability jumps to 75% when both parents have allergies, according to the Allergy & Asthma Network.
Allergies can develop at any point in life. Exposure to new environments or changes in one’s immune system can result in a new allergy in adulthood, for example common allergens that trigger an allergic response include:
As mentioned above, those with a family history of allergies are at a higher risk of developing allergies.
While many allergies develop during childhood, adults in their 20s and 30s are also at risk of developing allergies. Those with existing asthma are also at a higher risk of developing an allergy.
Family history of allergies
Adults in their 20s and 30s
Existing asthma
Diagnosing an allergy requires a doctor or an allergist. The medical professional will take a medical history of the patient, conduct a physical exam, and then administer specific tests based on which allergy is suspected.
AllerVie Health providers offer an assortment of testing, ranging from allergy patch testing to blood testing.

Skin Allergy Testing
This is less invasive than blood tests and is a good alternative for patients who don’t like needles.
learn more
Food Allergy Testing
A challenge test is a highly accurate diagnostic test to determine if a patient has outgrown a food allergy.
learn more
Blood Testing for Allergies
Blood tests can tell if someone has allergies by finding antibodies in the blood that react to allergens.
learn more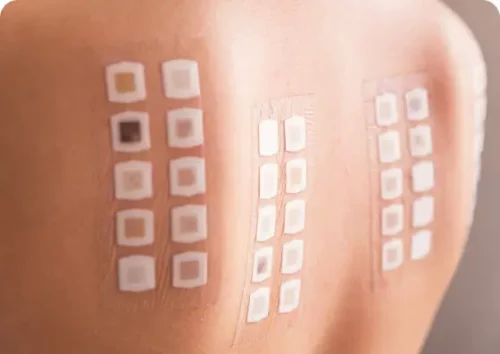
Allergy Patch Testing
Allergy patch testing is a common test used to confirm the cause of allergic contact dermatitis.
learn more
Intradermal Allergy Testing
This is done after a scratch test and involves injecting a small amount of an allergen under the skin.
learn more
Penicillin Allergy Testing
Most people who report a penicillin allergy actually had a one-time reaction and may be able to have penicillin again.
learn moreAlthough there’s no cure for allergies, there are several ways to treat allergy symptoms, including:
Several medications can be purchased over the counter, but some of the stronger medications will require a prescription from a medical provider. Mostly, patients can administer these common allergy treatments themselves.
Nasal Sprays
As the name suggests, this form of allergy treatment is sprayed directly into the nose. The three most common types of nasal sprays are:
Oral Corticosteroids
These medications, which can be taken in pill or liquid form, stop several allergic reactions and reduce swelling in the airways. They are powerful medications and require close supervision from the prescribing physician. This type of treatment can be an effective, short-term solution for people with severe allergies. Medical providers prescribe oral corticosteroids to treat swelling and inflammation usually associated with allergies. Common oral corticosteroids include methylprednisolone and prednisone.
Antihistamines
Antihistamines come in pill, liquid, tablet or spray form and work to block the release of histamines in the body. Histamines are chemicals that overreact to allergens they see as a threat, causing allergy symptoms such as coughing and sneezing. They are most commonly used to treat indoor or seasonal allergies. Antihistamines can be purchased over the counter but can also be prescribed by a medical provider. Most patients may be familiar with antihistamines in the form of diphenhydramine (or Benadryl®) and desloratadine (or Clarinex®). Mast cell stabilizers also stop the release of histamines and are used in eye drop or nose spray form.
Epinephrine
Epinephrine is delivered to the body via a self-injectable device loaded with a pre-measured dose. It is an essential tool in addressing anaphylaxis. Any patient at risk of anaphylaxis will typically carry one of these devices with them. Epinephrine is commonly used to treat those with insect, food, or drug allergies.
Corticosteroid Creams and Ointments
This kind of allergy treatment is used to make skin rashes that can be caused by allergies less itchy and less painful. Corticosteroid creams that are mild, like hydrocortisone skin cream, can be bought without a prescription. But stronger ones, like betamethasone, can only be bought with a prescription from a doctor.
Eye Drops for Allergies
These liquid medicines treat eye allergy symptoms, such as tearing, burning, and itchy eyes. Many eye drops are available over the counter, but if you need something stronger, you may need a prescription from a medical provider. These are the different kinds of eye drops for varying symptoms and allergens:
Immunotherapy helps get to the main reason for diseases by either turning up or turning down the immune response of the body. Through immunotherapy, small amounts of allergens are given to the body so that it “learns” not to react.
Immunotherapy can be taken by mouth, put under the tongue, or given as an injection. This treatment is often given in the form of allergy shots or allergy drops. Immunotherapy should be supervised by a doctor, since it can be complicated in the beginning.
Build-Up Stage
This stage takes anywhere from 3 to 6 months generally and involves getting the patient safely to the effective dose. Once reached, the process moves into the maintenance stage.
Maintenance Stage
During this stage, the patient takes the effective dose on an ongoing basis. This stage can last for an undesignated amount of time until a patient starts to experience prolonged relief.
Relief From Symptoms
After an initial improvement in symptoms, you may not notice additional improvement for several months. If successful, you should see long-term benefits and a reduction in symptoms.
Immunotherapy side effects
Be aware that side effects, such as allergy symptoms, can manifest in some patients. Anaphylaxis can occur in rare cases. However, at this time, there aren’t any known long-term side effects associated with this treatment.

Allergy shots are a very common form of immunotherapy and work similarly to a vaccine:
The body is exposed to small amounts of an allergen, allowing the body to gradually build up its immune response.
Patients get allergy shots, administered by a medical provider, one to two times a week during the initial stage of treatment, which can last between three and six months.
Appointments are quick, but patients will have to stick around for a few minutes to make sure there’s no adverse reaction. The maintenance phase can last between three and five years. Outcomes will vary from patient to patient.
Allergy shots can help treat:
Allergy drops, also called sublingual immunotherapy, are placed under the patient’s tongue.
These drops gradually expose the patient to small amounts of an allergen.
The long-term goal is for the immune system to become desensitized to this allergen, giving way to less severe symptoms.
Allergy drops are an excellent alternative option to allergy shots, whether you don’t like them, or they aren’t effective for you.
Allergy drops are currently only available in our Birmingham, AL clinics in Homewood, Hoover, Oxford, and Cullman.
Not all treatments and special programs are offered at every AllerVie location or by every AllerVie provider. If your provider does administer allergy drops, they can help treat:

The first appointment will take the longest: There’s a 30-minute monitoring period after the drops are administered. This is a safety measure to ensure that the patient gets medical help if needed. Patients who tolerate the stop well during the first visit will self-administer future doses at home.

Oral immunotherapy, or OIT, is when a patient is slowly and methodically exposed to a food allergy while being watched by a doctor.
At first, the patient eats or drinks far less of the allergen than would normally cause an allergic response. Over time, the doctor will increase the dose, and the patient will also need to take a dose every day at home.
OIT has a lot of benefits for people who are allergic to popular foods like peanuts or tree nuts that are hard to avoid. It can take time, though, and the patient has to keep following maintenance procedures.
Most people hit the maintenance stage in four to six months. OIT can reduce the chance that a patient will have a serious or fatal allergic reaction, but it needs to be maintained for the rest of the patient’s life.
Any patient who experiences chronic allergy symptoms should see a doctor or allergist. However, an allergist could be especially helpful to patients who have allergy symptoms that interfere with their quality of life or who experience seasonal allergy symptoms several months throughout the year.
With board-certified allergists across the United States, AllerVie Health can help you find relief from chronic allergy symptoms.
Common, recurring symptoms that you can experience can include:
Currently, there isn’t a cure for allergies—despite the condition’s widespread reach. But there are several ways to lessen the chronic burden allergies can leave behind, including: