
 go back
go back
Eosinophilic Esophagitis
In EoE, esophageal inflammation interferes with eating and digesting. EoE is more widespread today due to improved medical awareness and allergies and asthma.
Make An AppointmentWhat is Eosinophilic Esophagitis?
Eosinophilic esophagitis, or EoE, is an immune and allergy disorder of the esophagus.
In EoE, the patient experiences inflammation in the esophagus that interferes with their ability to ingest and digest food. Cases of EoE are more common today, due in part to increased physician awareness and in part to an uptick in allergies and asthma. It is a chronic condition, but can be managed medically in the long term.
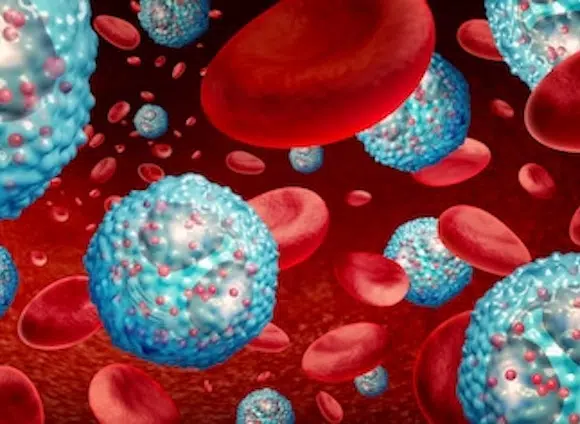
In EoE, the patient has a high number of white blood cells known as eosinophils in the esophagus that trigger inflammation. These cells are typically not present in the esophagus. The esophagus swells as a result, making it difficult for the patient to pass swallowed food through the esophagus.
01
Severe Cases
In severe cases of EoE, the patient can experience what is known as a “food impaction.” In a food impaction, the esophagus has narrowed so much that food becomes entirely stuck and builds up. If the patient is unable to swallow or vomit up the food, they will need emergency medical attention.
02
Stages
EoE can look very different at different stages of life. In infants, the disease can result in an aversion to eating; as a result, the child may not meet typical growth milestones. In school-age children, the patient may have abdominal pain, trouble swallowing, and vomit often. In teens and adults often have difficulty swallowing dry foods.
Signs & Symptoms of Eosinophilic Esophagitis
The signs and symptoms of EoE vary from patient to patient and from one age group to the next. Patients with EoE can experience any combination of the following symptoms:
- Dysphagia, or difficulty swallowing
- Food impaction
- Regurgitation
- Nausea
- Vomiting
- Stomach pain
- Loss of appetite
- Malnutrition
*Note: Patients may also experience a centralized pain in the chest that does not respond to taking antacids. Any patient experiencing symptoms of EoE should consult with a physician.
What Causes Eosinophilic Esophagitis?
EoE is caused by the presence of a high volume of eosinophils in the esophagus. There are several different things that may trigger this. Patients with a family history of EoE are more likely to develop the condition, for one. EoE patients are often atopic, as well, meaning they have one or more allergies.
Asthma patients are also at a higher risk of developing EoE. Finally, those who love in a cold or dry climate are also at a higher risk.
HOW EOSINOPHILIC ESOPHAGITIS IS DIAGNOSED
Diagnosing EoE requires a gastroenterologist. Since many patients with EoE have allergies, they typically are referred to a gastroenterologist by their allergist. A gastroenterologist who suspects EoE may also refer a patient to an allergist, if they are not currently seeing one. EoE diagnosis can involve several tests, each of which is detailed below.
Endoscopy
- Conducting an upper endoscopy is the primary method used to diagnose EoE. In this procedure, the doctor inserts a flexible tube with a light source into the esophagus. This allows the doctor to observe the esophagus and any areas of inflammation. During this process, the doctor also takes small biopsies of the esophageal tissue.
- An endoscopy with biopsies is a very safe procedure. In rare cases, patients may experience complications, including infection or bleeding. The best way to reduce complications is to follow physician instructions before the procedure.
Esophageal Mucosal Biopsy
- As mentioned above, the upper endoscopy also includes taking several biopsies of the mucosal lining of the esophagus. This is a simple and safe procedure. The doctor passes specialized, surgical tools through the flexible tube in the throat and uses these to extract the tissue samples. A video monitor helps guide the process.
- Either the doctor or a pathologist will then examine the tissue samples under a microscope to look for the presence of eosinophils. Test results from a laboratory can take a few days.
Allergy Assessment
- Your doctor may also recommend an allergy assessment done with an allergist. Allergy assessment for EoE can involve a number of tests, including a skin tests such as skin prick and patch tests, and blood tests that include serum testing.
- In a skin prick test, a small sample of an allergen is swabbed onto the skin. The doctor then pricks the top layer of the skin, exposing it to the allergen and looks for a reaction. A patch test follows similar principles and can be better at assessing the delayed allergic reactions associated with EoE.
- Finally, a patient may also undergo serum testing to diagnose allergies associated with EoE. Serum testing involves taking samples of blood and determining the level of IgE in the blood after exposure to an allergen.
Diagnostic Criteria
- When diagnosing EoE, three criteria must be met:
There must be clinical symptoms of dysfunction in the esophagus, an esophageal biopsy must show at least 15 eosinophils per microscopy field, and the diagnosing physician must rule out other possible causes.
Treatments for Eosinophilic Esophagitis
There is no known cure for eosinophilic esophagitis. There are, however, several treatments that can ameliorate symptoms and help a patient manage the condition in the long term.
Dietary Management
Dietary management for EoE works by limiting the patient’s exposure to any allergy triggers. The design of a patient’s dietary therapy for EoE will depend in large part to the results of their allergy assessment.
A dietary management plan for EoE can involve a good number of restrictions and limitations. Patients should work to avoid foods, such as dairy or wheat, for example, that may exacerbate symptoms and inflammation. The doctor will work in close consultation with the patient to develop a plan that balances clinical need with the patient’s lifestyle.
Medications
There are two primary medications used in the treatment of EoE. Doctors will prescribe both or either of these medications in close consultation with the patient. EoE medications require ongoing medication management.
A primary line of defense with EoE is the Protein Pump Inhibitor, or PPO. This medication is a n acid blocker and easy for patients to use, but does not result in significant improvement of symptoms in the majority of cases.
As such, many doctors also prescribe topical steroids to treat EoE. Steroids such as budesonide or fluticasone, come in liquid forms that can be easily swallowed by the patient. Since the steroid is ingested through the digestive system, it does not get into the bloodstream, allowing patients to avoid many of the side effects associated with topical steroids.
Endoscopic Dilatation
In situations where steroids have not worked or a patient is experiencing a severe stricture in the esophagus, a doctor may recommend endoscopic dilatation. This medical procedure involves stretching the interior of the esophagus to facilitate swallowing.
Endoscopic dilatation may involve sedation to help a patient relax. The doctor may also spray the patient’s throat with anesthetic spray, then pass an endoscopic tube into the esophagus. Either a plastic dilator or a dilating balloon will then be used to stretch out the esophagus.
Patients may feel some tension and pressure in the back of the throat during the process.
Recovery from a dilatation is relatively quick. Patients who have received sedation will be observed for a period of time after the procedure.
